What is Palliative Care? Myths, misconceptions and musings
Palliative care can sometimes feel a bit elusive in the world of healthcare. It sounds like a nice, “soft” word and at the very least most people have a vague association of it with comfort care. But what is it, really?
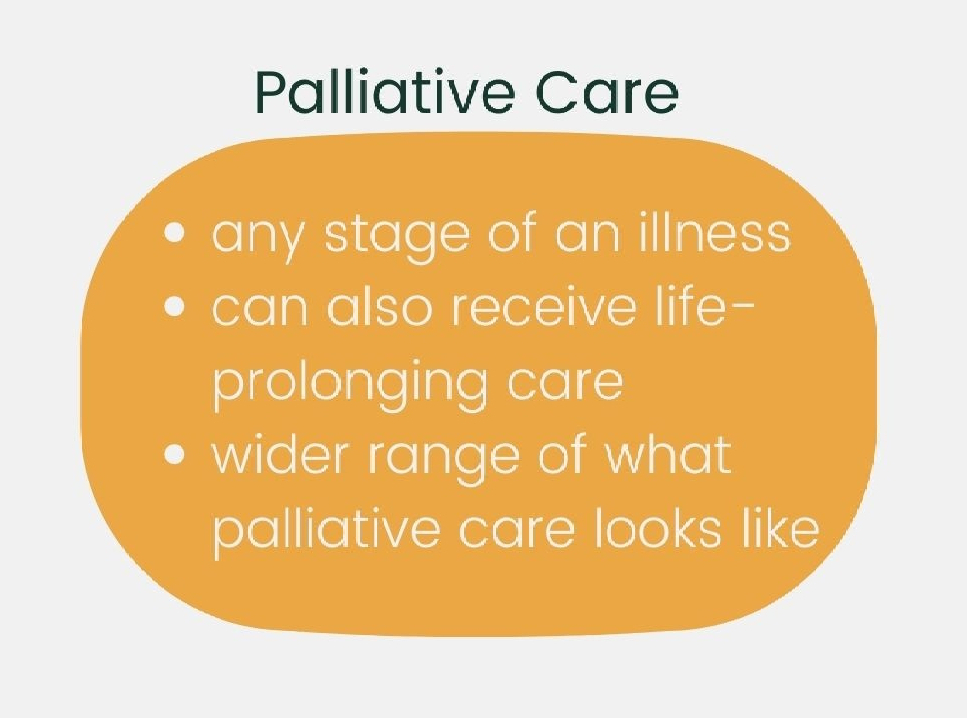
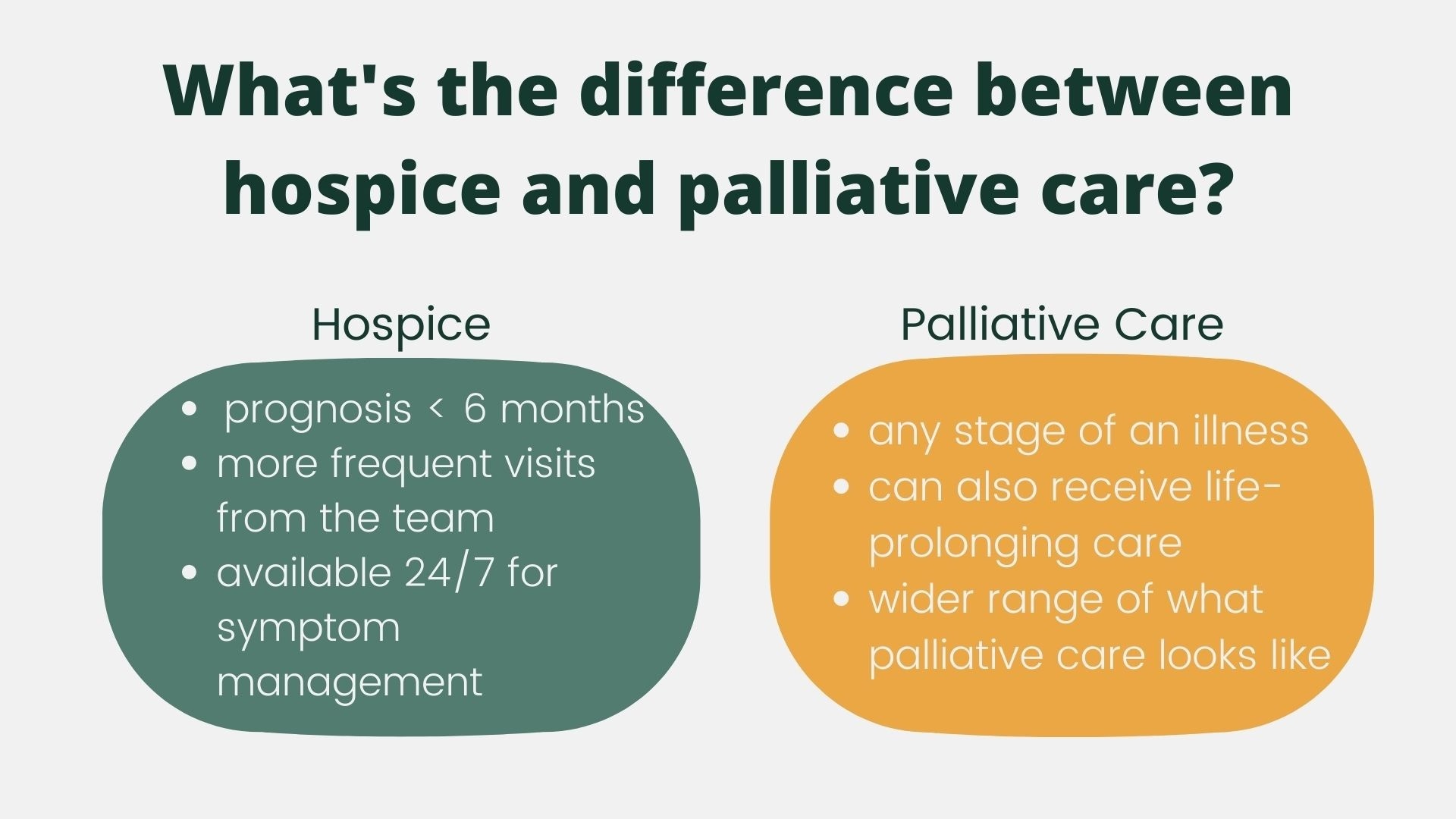
Sometimes “palliative care” gets thrown around with “hospice care” or even used as a complete substitution. Other times, even healthcare workers have a hard time describing it because the care can vary widely–everything from a one-time consult to outpatient-based care to a full blown robust program offering a variety of providers for in-home support.
So let’s jump in! Despite the wide variety of what palliative care can look like, all palliative programs align in several key areas.
Here’s what palliative care is NOT:
➡️ Palliative care is not always “pre-hospice”. Palliative care is for someone of ANY age at ANY stage of a serious illness.
➡️ Palliative care shouldn’t just be used as a “softer” way to suggest comfort care when someone is at the end stage of a disease and hospice eligible.
This one has a lot wrapped up into it. Doctors and other healthcare workers sometimes struggle with end of life discussions. Heck, it’s not easy, even if it’s your everyday work! Doctors are also under a lot of pressure (from society and from patients) to not be perceived as “giving up” on someone. Unfortunately, sometimes this can delay conversations when they’re needed most. At times, suggesting palliative care to a person can be an easy way out for healthcare workers who struggle with the conversation, but we can do better than that. (Palliative care IS appropriate for someone who is hospice eligible, but isn’t yet ready mentally/emotionally/spiritually for hospice.)
➡️ Palliative care isn’t just for when someone is having unmanaged pain. Palliative care helps to manage any symptoms someone may be experiencing as a result of an illness (or treatments of an illness, like side effects from chemo).
Palliative care workers also help someone to define and express what’s important in their healthcare, find meaning in life and in illness, cope with spiritual and emotional distress from an illness, and yes—plan for the care someone wants as their illness progresses.
The reality is–palliative care doesn’t have to be scary and it isn’t hospice in disguise. Whether you realize it or not, you make decisions from a palliative care lens all the time. Maybe you have a new ache in your side or a nagging reminder that your teeth cleaning is overdue–With each health-related issue that surfaces, you weigh how much it impacts your everyday life in the context of other things that are vying for your attention. When a doctor tells you to quit smoking, lose weight, or get a medical test done, you weigh the benefit vs. burden and decide how soon to follow through, or if you want to follow through at all.
So let’s revisit our initial question: What IS palliative care?
Palliative care IS:
➡️ Support in making intentional healthcare decisions aligned with what’s important to you
➡️ Holistic symptom management, taking into account your physical, emotional, and spiritual needs
➡️ A collaborative approach with your palliative care team, your primary care doctor and any speciality doctors, your loved ones (if you so choose) and YOU.
We’ve only just scratched the surface! Curious about what factors contribute to accessing palliative care, when you should seek it out, and how care can look different across different programs? Stay tuned.
Ready to continue the conversation now about your individual health needs? Reach out to set up your first health counseling session.